Danh mục
A spinal cord injury (SCI) is damage to any part of the spinal cord or nerves at the end of the spinal canal. The condition often causes permanent changes in strength, sensation, and other body functions below the site of the injury.
Motor vehicle accidents, acts of violence, and sporting injuries are the common causes of spinal cord injury (SCI). The mechanism of injury influences the type of SCI and the degree of neurological deficit. Spinal cord lesions are classified as a complete (total loss of sensation and voluntary motor function) or incomplete (mixed loss of sensation and voluntary motor function).
Physical findings vary, depending on the level of injury, degree of spinal shock, and phase and degree of recovery, but in general, are classified as follows:
Nursing care planning and goals for patients with spinal cord injuries includes: maximizing respiratory function, preventing injury to the spinal cord, promote mobility and/or independence, prevent or minimize complications, support psychological adjustment of patient and/or SO, and providing information about the injury, prognosis, and treatment.
Here are 12 nursing care plans for patients with spinal cord injury:
Risk for Ineffective Breathing Pattern: The state in which an individual is at high risk to experience an actual or potential loss of adequate ventilation.
Risk factors may include
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Assess respiratory function by asking patient to take a deep breath. Note presence or absence of spontaneous effort and quality of respirations (labored, using accessory muscles). | C-1 to C-3 injuries result in complete loss of respiratory function. Injuries at C-4 or C-5 can lead to variable loss of respiratory function, depending on phrenic nerve involvement and diaphragmatic function, but generally cause decreased vital capacity and inspiratory effort. For injuries below C-6 or C-7, respiratory muscle function is preserved; however, weakness or impairment of intercostal muscles may impair effectiveness of cough and the ability to sigh, deep breathe. |
| Auscultate breath sounds. Note areas of absent or decreased breath sounds or development of adventitious sounds (rhonchi). | Hypoventilation is common and leads to accumulation of secretions, atelectasis, and pneumonia (frequent complications). Note: Respiratory compromise is one of the leading causes of mortality, especially during the acute stage as well as later in life. |
| Note strength or effectiveness of cough. | Level of injury determines the function of intercostal muscles and ability to cough spontaneously or move secretions. |
| Observe skin color for developing cyanosis, duskiness. | May reveal impending respiratory failure, need for immediate medical evaluation and intervention. |
| Assess for abdominal distension and muscle spasm. | Abdominal fullness may impede diaphragmatic excursion, reducing lung expansion and further compromising respiratory function. |
| Monitor and limit visitors as indicated. | General debilitation and respiratory compromise place patient at increased risk for acquiring URIs. |
| Monitor diaphragmatic movement when phrenic pacemaker is implanted. | Stimulation of phrenic nerve may enhance respiratory effort, decreasing dependency on mechanical ventilator. |
| Elicit concerns and questions regarding mechanical ventilation devices. | Acknowledges reality of situation. |
| Provide honest answers. | Future respiratory function needs will not be totally known until spinal shock resolves and acute rehabilitative phase is completed. Even though respiratory support may be required, alternative devices and techniques may be used to enhance mobility and promote independence. |
| Maintain patent airway: keep head in neutral position, elevate head of bed slightly if tolerated, use airway adjuncts as indicated. | Patients with high cervical injury and impaired gag and cough reflexes require assistance in preventing aspiration and maintaining patient airway. |
| Assist patient in “taking control” of respirations as indicated. Instruct in and encourage deep breathing, focusing attention on steps of breathing. | Breathing may no longer be a totally voluntary activity but require conscious effort, depending on level of injury and involvement of respiratory muscles. |
| Assist with coughing as indicated for level of injury (have patient take deep breath and hold for 2 sec before coughing, or inhale deeply, then cough at the end of a slow exhalation). Alternatively, assist by placing hands below diaphragm and pushing upward as patient exhales (quad cough). | Adds volume to cough and facilitates expectoration of secretions or helps move them high enough to be suctioned out. Note: Quad cough procedure is generally reserved for patients with stable injuries once they are in the rehabilitation stage. |
| Suction as necessary. Document quality and quantity of secretions. | If cough is ineffective, suctioning may be needed to remove secretions, enhance gas exchange, and reduce risk of respiratory infections. Note: “Routine” suctioning increases risk of hypoxia, bradycardia (vagal response), tissue trauma. Therefore, suctioning needs are based on inability to move secretions. |
| Reposition and turn periodically. Avoid and limit prone position when indicated. | Enhances ventilation of all lung segments, mobilizes secretions, reducing risk of complications such as atelectasis and pneumonia. Note: Prone position significantly decreases vital capacity, increasing risk of respiratory compromise and failure. |
| Encourage fluids (at least 2000 mL per day). | Aids in liquefying secretions, promoting mobilization and expectoration. |
| Measure or graph: | |
|
Determines level of respiratory muscle function. Serial measurements may be done to predict impending respiratory failure (acute injury) or determine level of function after spinal shock phase and while weaning from ventilatory support. |
|
Documents status of ventilation and oxygenation, identifies respiratory problems such as hypoventilation (low Pao2and elevated Paco2) and pulmonary complications. |
| Administer oxygen by appropriate method (nasal prongs, mask, intubation, ventilator). | Method is determined by level of injury, degree of respiratory insufficiency, and amount of recovery of respiratory muscle function after spinal shock phase. |
| Assist with use of respiratory adjuncts (incentive spirometer, blow bottles) and aggressive chest physiotherapy (chest percussion). | Preventing retained secretions is essential to maximize gas diffusion and to reduce risk of pneumonia. |
| Refer and consult with respiratory and physical therapists. | Helpful in identifying exercises individually appropriate to stimulate and strengthen respiratory muscles and effort. For example, glossopharyngeal breathing uses muscles of mouth, pharynx, and larynx to swallow air into lungs, thereby enhancing VC and chest expansion. |
Tin tức mới nhất
Sử dụng paracetamol dạng truyền tĩnh mạch (1 gram/100 mL)
DỰ THẢO VĂN KIỆN ĐẠI HỘI ĐẠI BIỂU KHÓA III, NHIỆM KỲ 2024 -2029
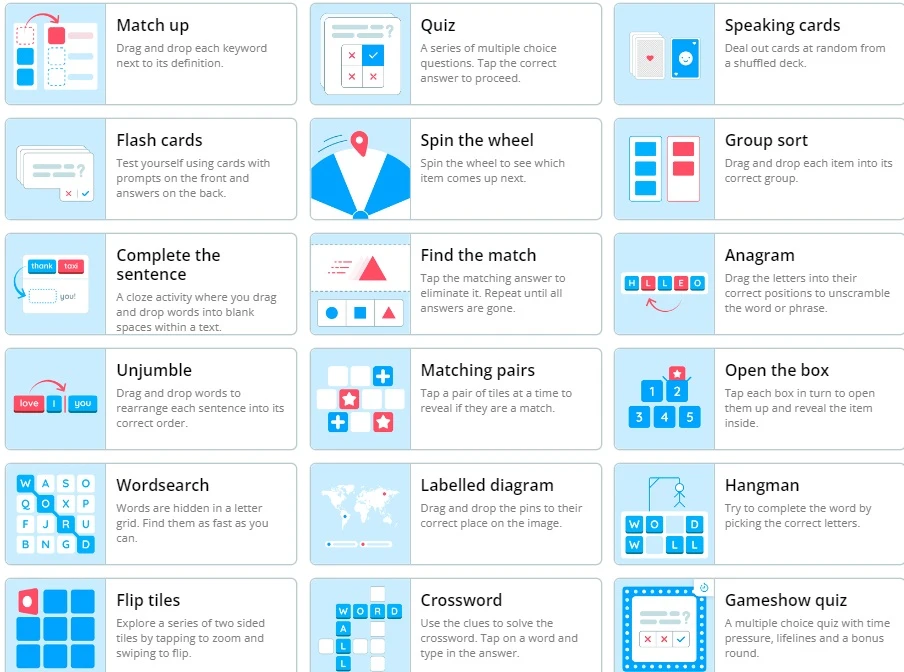
Wordwall là một công cụ dạy học trực tuyến
2 Diagnostics infirmiers NANDA 2021 -2023

Kỷ yếu hội nghị Điều dưỡng Bệnh viện HN Việt Đức 2022
Sample size calculator
Nghiên cứu bắt đầu từ đâu
Học thống kê với Dr Nuc
Hồi quy và tương quan
học Spss
địa chỉ open journal

Phần mềm điện thoại nursing