Danh mục
Peritonitis is the acute or chronic inflammation of the peritoneum, the membrane that lines the abdominal cavity and covers the visceral organs. Inflammation may extend throughout the peritoneum or may be localized as an abscess. Peritonitis commonly decreases intestinal motility and causes intestinal distention with gas. mortality is 10% with death usually a result of bowel obstruction.
The peritoneum is sterile, despite the GI tract normally contains bacteria. When bacteria invade the peritoneum due to an inflammation or perforation of the GI tract peritonitis usually occurs. Bacterial invasion usually results from appendicitis, diverticulitis, peptic ulcer, ulcerative colitis, volvulus, abdominal neoplasms, or a stab wound. It may also be associated with peritoneal dialysis.
Early treatment of GI inflammation conditions and preoperative and postoperative therapy help prevent peritonitis. Patient care includes monitoring and measures to prevent complications and the spread of infection. Here are 6 peritonitis nursing care plans.
Nursing Diagnosis
Risk factors may include
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Note individual risk factors. Abdominal trauma, acute appendicitis, peritoneal dialysis are common risk factors. | Influences choice of interventions. |
| Assess vital signs frequently, noting unresolved or progressing hypotension, decreased pulse pressure, tachycardia, fever, tachypnea. | Signs of impending septic shock. Circulating endotoxins eventually produce vasodilation, shift of fluid from circulation, and a low cardiac output state. |
| Note changes in mental status: confusion, stupor, altered LOC. | Hypoxemia, hypotension, and acidosis can cause deteriorating mental status. |
| Note skin color, temperature, moisture. | Warm, flushed, dry skin is early sign of septicemia. Later manifestations include cool, clammy, pale skin and cyanosis as shock becomes refractory. |
| Monitor urine output. | Oliguria develops as a result of decreased renal perfusion, circulating toxins, effects of antibiotics. |
| Maintain strict aseptic technique in care of abdominal drains, incisions and/or open wounds, dressings, and invasive sites. Cleanse with appropriate solution. | Prevents access or limits spread of infecting organisms and cross-contamination. |
| Perform and teach proper hand washing technique. | Reduces risk of cross-contamination and/or spread of infection. |
| Observe drainage from wounds and/or drains. | Provides information about status of infection. |
| Maintain sterile technique when catheterizing patient, and provide catheter care and encourage perineal cleansing on a routine basis. | Prevents access, limits bacterial growth in urinary tract. |
| Monitor and/or restrict visitors and staff as appropriate. Provide protective isolation if indicated. | Reduces risk of exposure to and/or acquisition of secondary infection in immuno compromised patient. |
| Obtain specimens and monitor results of serial blood, urine, wound cultures. | Identifies causative microorganisms and helps in assessing effectiveness of antimicrobial regimen. |
| Assist with peritoneal aspiration, if indicated. | May be done to remove fluid and to identify infecting organisms so appropriate antibiotic therapy can be instituted. |
| Administer antimicrobials: gentamicin (Garamycin), amikacin (Amikin), clindamycin (Cleocin), via IV/peritoneal lavage. | Therapy is directed at anaerobic bacteria and aerobic Gram-negative bacilli. Lavage may be used to remove necrotic debris and treat inflammation that is poorly localized or diffused. |
| Prepare for surgical intervention if indicated. | Surgery may be treatment of choice (curative) in acute, localized peritonitis, e.g., to drain localized abscess; remove peritoneal exudates, ruptured appendix or gallbladder; plicate perforated ulcer; or resect bowel. |
Nursing Diagnosis:
May be related to
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Monitor vital signs, noting presence of hypotension (including postural changes), tachycardia, tachypnea, fever. Measure central venous pressure (CVP) if available. | Aids in evaluating degree of fluid deficit or effectiveness of fluid replacement therapy and response to medications. |
| Maintain accurate I&O and correlate with daily weights. Include measured losses. Include measurements from gastric suction, drains, dressings, Hemovacs, diaphoresis, and abdominal girth for third spacing of fluid. | Reflects overall hydration status. Urine output may be diminished because of hypovolemia and decreased renal perfusion, but weight may still increase, reflecting tissue edema or ascites accumulation. Gastric suction losses may be large, and a great deal of fluid can be sequestered in the bowel and peritoneal space (ascites). |
| Measure urine specific gravity. | Reflects hydration status and changes in renal function, which may warn of developing acute renal failure in response to hypovolemia and effect of toxins. Many antibiotics also have nephrotoxic effects that may further affect kidney function and urine output. |
| Observe skin or mucous membrane dryness, turgor. Note peripheral and sacral edema. | Hypovolemia, fluid shifts, and nutritional deficits contribute to poor skin turgor, taut edematous tissues. |
| Eliminate noxious sights and smells from environment. Limit intake of ice chips. | Reduces gastric stimulation and vomiting response. Excessive use of ice chips during gastric aspiration can increase gastric washout of electrolytes. |
| Change position frequently, provide frequent skin care, and maintain dry or wrinkle-free bedding. | Edematous tissue with compromised circulation is prone to breakdown. |
| Monitor laboratory studies: Hb/ Hct, electrolytes, protein, albumin, BUN, Cr. | Provides information about hydration, organ function. Varied alterations with significant consequences to systemic function are possible as a result of fluid shifts, hypovolemia, hypoxemia, circulating toxins, and necrotic tissue products. |
| Administer plasma or blood, fluids, electrolytes, diuretics as indicated. | Replenishes circulating volume and electrolyte balance. Colloids (plasma, blood) help move water back into intravascular compartment by increasing osmotic pressure gradient. Diuretics may be used to assist in excretion of toxins and to enhance renal function. |
| Maintain NPO with nasogastric or intestinal aspiration. | Reduces hyperactivity of bowel and diarrhea losses. |
May be related to
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Investigate pain reports, noting location, duration, intensity(0–10 scale), and characteristics (dull, sharp, constant). | Changes in location or intensity are not uncommon but may reflect developing complications. Pain tends to become constant, more intense, and diffuse over the entire abdomen as inflammatory process accelerates; pain may localize if an abscess develops. |
| Maintain semi-Fowler’s position as indicated. | Facilitates fluid or wound drainage by gravity, reducing diaphragmatic irritation and/or abdominal tension, and thereby reducing pain. |
| Move patient slowly and deliberately, splinting painful area. | Reduces muscle tension and guarding, which may help minimize pain of movement. |
| Provide comfort measures: massage, back rubs, deep breathing. Instruct in relaxation and visualization exercises. Provide diversional activities. | Promotes relaxation and may enhance patient’s coping abilities by refocusing attention. |
| Provide frequent oral care. Remove noxious environmental stimuli. | Reduces nausea and vomiting, which can increase intra-abdominal pressure and pain. |
| Administer medications as indicated: | |
| Analgesics, narcotics; | Reduce metabolic rate and intestinal irritation from circulating or local toxins, which aids in pain relief and promotes healing. Pain is usually severe and may require narcotic pain control. Analgesics may be withheld during initial diagnostic process because they can mask signs and symptoms. |
| Antiemetics: hydroxyzine (Vistaril); | Reduce nausea and vomiting, which can increase abdominal pain. |
| Antipyretics: acetaminophen (Tylenol). | Reduce discomfort associated with fever. |
Nursing Diagnosis
Risk factors may include
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Auscultate bowel sounds, noting absent or hyperactive sounds. | Although bowel sounds are frequently absent, inflammation and irritation of the intestine may be accompanied by intestinal hyperactivity, diminished water absorption, and diarrhea. |
| Monitor NG tube output. Note presence of vomiting, diarrhea. | Large amounts of gastric aspirant and vomiting and diarrhea suggest bowel obstruction, requiring further evaluation. |
| Measure abdominal girth. | Provides quantitative evidence of changes in gastric or intestinal distension and/or accumulation of ascites. |
| Assess abdomen frequently for return to softness, reappearance of normal bowel sounds, and passage of flatus. | Indicates return of normal bowel function and ability to resume oral intake. |
| Weigh regularly. | Initial losses or gains reflect changes in hydration, but sustained losses suggest nutritional deficit. |
| Monitor BUN, protein, prealbumin and albumin, glucose, nitrogen balance as indicated. | Reflects organ function and nutritional status and needs. |
| Advance diet as tolerated. Advance from clear liquids to soft food. | Careful progression of diet when intake is resumed reduces risk of gastric irritation. |
| Administer TPN as indicated. | Promotes nutrient utilization and positive nitrogen balance in patients who are unable to assimilate nutrients in a normal fashion. |
Nursing Diagnosis
May be related to
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Evaluate anxiety level, noting patient’s verbal and nonverbal response. Encourage free expression of emotions. | Apprehension may be escalated by severe pain, increasingly ill feeling, urgency of diagnostic procedures, and possibility of surgery. |
| Provide information regarding disease process and anticipated treatment. | Knowing what to expect can reduce anxiety. |
| Schedule adequate rest and uninterrupted periods for sleep. | Limits fatigue, conserves energy, and can enhance coping ability. |
Nursing Diagnosis:
May be related to
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Review underlying disease process and recovery expectations. | Provides knowledge base from which patient can make informed choices. |
| Identify signs and symptoms requiring medical evaluation: recurrent abdominal pain and distension, vomiting, fever, chills, or presence of purulent drainage, swelling, erythema of surgical incision (if present). | Early recognition and treatment of developing complications may prevent more serious illness and injury. |
| Discuss medication regimen, schedule, and possible side effects. | Antibiotics may be continued after discharge, depending on length of stay. |
| Recommend gradual resumption of usual activities as tolerated, allowing for adequate rest. | Prevents fatigue, enhances feeling of well-being. |
| Review activity restrictions or limitations: avoid heavy lifting, constipation. | Avoids unnecessary increase of intra-abdominal pressure and muscle tension. |
| Demonstrate aseptic dressing change, wound care. | Reduces risk of contamination. Provides opportunity to evaluate healing process. |
| Emphasize importance of medical follow-up. | Necessary to monitor resolution of infection and resumption of usual activities. |
Tin tức mới nhất
Sử dụng paracetamol dạng truyền tĩnh mạch (1 gram/100 mL)
DỰ THẢO VĂN KIỆN ĐẠI HỘI ĐẠI BIỂU KHÓA III, NHIỆM KỲ 2024 -2029
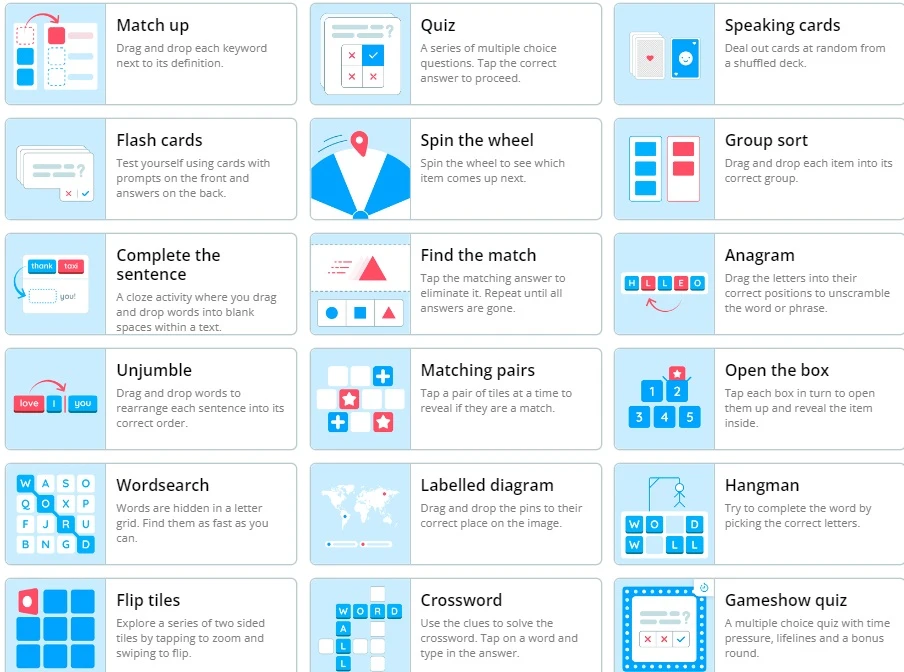
Wordwall là một công cụ dạy học trực tuyến
2 Diagnostics infirmiers NANDA 2021 -2023

Kỷ yếu hội nghị Điều dưỡng Bệnh viện HN Việt Đức 2022
Sample size calculator
Nghiên cứu bắt đầu từ đâu
Học thống kê với Dr Nuc
Hồi quy và tương quan
học Spss
địa chỉ open journal

Phần mềm điện thoại nursing