Danh mục
The intraoperative phase extends from the time the client is admitted to the operating room, to the time of anesthesia administration, performance of the surgical procedure and until the client is transported to the recovery room or postanesthesia care unit (PACU).
Throughout the surgical experience the nurse functions as the patient’s chief advocate. The nurse’s care and concern extend from the time the patient is prepared for and instructed about the forthcoming surgical procedure to the immediate preoperative period and into the operative phase and recovery from anesthesia. The patient needs the security of knowing that someone is providing protection during the procedure and while he is anesthetized because surgery is usually a stressful experience.
The intraoperative phase begins when the patient is received in the surgical area and lasts until the patient is transferred to the recovery area. Although the surgeon has the most important role in this phase, there are key members of the surgical team.
The circulating nurse manages the operating room and protects the safety and health needs of the patient by monitoring activities of members of the surgical team and checking the conditions in the operating room. Responsibilities of a circulation nurse are the following:
The scrub nurse assists the surgeon during the whole procedure by anticipating the required instruments and setting up the sterile table. The responsibilities of the scrub nurse are:
Classification of Physical Status for Anesthesia Before Surgery
The anesthesiologist should visit the patient before the surgery to provide information, answer questions and allay fears that may exist in the patient’s mind.
The choice of anesthetic agent will be discussed and the patient has an opportunity to disclose and the patient has opportunity to disclose previous reactions and information about any medication currently being taken that may affect the choice of an agent. Aside from that, the patient’s general condition must also be assessed because it may affect the management of anesthesia. Thus, the anesthesiologist assesses the patient’s cardiovascular system and lungs.
Inquiry about preexisting pulmonary infection sand the extent to which the patient smokes must also be determined. The classification of a client’s physical status for anesthesia before surgery is summarized below.
| Classification of Physical Status for Anesthesia Before Surgery | ||
| Classification | Description | Example |
| Good | No organic disease; no systemic disturbance | Uncomplicated hernias, fracture |
| Fair | Mild to moderate systemic disturbance | Mild cardiac (I and II) disease, mild diabetes |
| Poor | Severe systemic disturbance | Poorly controlled diabetes, pulmonary complications, moderate cardiac (III) disease |
| Serious | Systemic disease threatening life | Severe renal disease, severe cardiac disease (IV), decompensation |
| Moribund | Little chance of survival but submitting to operation in desperation | Massive pulmonary embolus, ruptured abdominal aneurysm with profound shock |
| Emergency | Any of the above when surgery is performed in an emergency situation | An uncomplicated hernia that is now strangulated and associated with nausea and vomiting. |
Source: Brunner and Suddarth’s Medical-Surgical Nursing by Smeltzer and Bare
Anesthesia controls pain during surgery or other medical procedures. It includes using medicines, and sometimes close monitoring, to keep you comfortable. It can also help control breathing, blood pressure, blood flow, and heart rate and rhythm, when needed. Anesthetics are divided into two classes:
This type of anesthesia promotes total loss of consciousness and sensation. General anesthesia is commonly achieved when the anesthetic is inhaled or administered intravenously. It affects the brain as well as the entire body. Types of general anesthesia administration:
Volatile liquid anesthetics – this type of anesthetic produces anesthesia when their vapors are inhaled. Included in this group are the following:
Gas Anesthetics – anesthetics administered by inhalation and are ALWAYS combined with oxygen. Included in this group are the following:
Stages
General anesthesia consists of four stages, each of which presents a definite group of signs and symptoms.
Stage I: Onset or Induction or Beginning anesthesia.
This stage extends from the administration of anesthesia to the time of loss of consciousness. The patient may have a ringing, roaring or buzzing in the ears and though still conscious, is aware of being unable to move the extremities easily. Low voices or minor sounds appear distressingly loud and unreal during this stage.
Stage II: Excitement or Delirium.
Stage II extends from the time of loss of consciousness to the time of loss of lid reflex. This stage is characterized by struggling, shouting, talking, singing, laughing or even crying. However, these things may be avoided if the anesthetic is administered smoothly and quickly. The pupils become dilated but contract if exposed to light. Pulse rate is rapid and respirations are irregular.
Stage III: Surgical Anesthesia.
This stage extends from the loss of lid reflex to the loss of most reflexes. It is reached by continued administration of the vapor or gas. The patient now is unconscious and is lying quietly on the table. Respirations are regular and the pulse rate is normal.
Stage IV: Overdosage or Medullary or Stage of Danger.
This stage is reached when too much anesthesia has been administered. It is characterized by respiratory or cardiac depression or arrest. Respirations become shallow, the pulse is weak and thread and the pupils are widely dilated and no longer contract when exposed to light. Cyanosis develops afterwards and death follows rapidly unless prompt action is taken. To prevent death, immediate discontinuation of anesthetic should be done and respiratory and circulatory support is necessary.
Local anesthetics can be topical, or isolated just to the surface. These are usually in the form of gels, creams or sprays. They may be applied to the skin before the injection of a local anesthetic that works to numb the area more deeply, in order to avoid the pain of the needle or the drug itself (penicillin, for example, causes pain upon injection).
Regional anesthesia blocks pain to a larger part of the body. Anesthetic is injected around major nerves or the spinal cord. Medications may be administered to help the patient relax or sleep. Major types of regional anesthesia include:
With regional anesthesia, an anesthetic agent is injected around the nerved so that the area supplied by these nerves is anesthetized. The effect depends on the type of nerve involved. The patient under a spinal or local anesthesia is awake and aware of his or her surroundings.
Regional anesthesia carries more risks than local anesthesia, such as seizures and heart attacks, because of the increased involvement of the central nervous system. Sometimes regional anesthesia fails to provide enough pain relief or paralysis, and switching to general anesthesia is necessary.
This is a type of conduction nerve block that occurs by introducing a local anesthetic into the subarachnoid space at the lumbar level which is usually between L4 and L5. Sterile technique is used as the spinal puncture is made and medication is injected through the needle. The spread of the anesthetic agent and the level of anesthesia depend on:
The following are nursing assessment after anesthesia:
How do anesthesiologists determine the type of anesthesia to be used?
The type of anesthesia the anesthesiologist chooses depends on many factors. These include the procedure the client is having and his or her current health.
The nurse should have an idea which patient position is required for a certain surgical procedure to be performed. There are lots of factors to consider in positioning the patient which includes the following:
Here are the nursing responsibilities during intraoperative phase:
Tin tức mới nhất
Sử dụng paracetamol dạng truyền tĩnh mạch (1 gram/100 mL)
DỰ THẢO VĂN KIỆN ĐẠI HỘI ĐẠI BIỂU KHÓA III, NHIỆM KỲ 2024 -2029
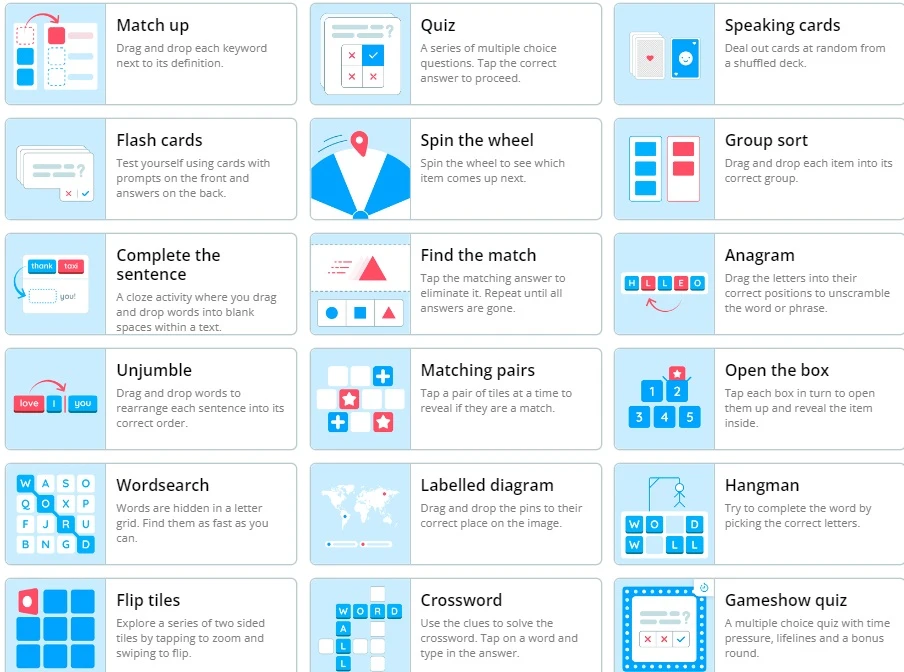
Wordwall là một công cụ dạy học trực tuyến
2 Diagnostics infirmiers NANDA 2021 -2023

Kỷ yếu hội nghị Điều dưỡng Bệnh viện HN Việt Đức 2022
Sample size calculator
Nghiên cứu bắt đầu từ đâu
Học thống kê với Dr Nuc
Hồi quy và tương quan
học Spss
địa chỉ open journal

Phần mềm điện thoại nursing