Danh mục

Total Parenteral Nutrition (TPN) is a method of administration of essential nutrients to the body through a central vein. TPN therapy is indicated to a client with a weight loss of 10% the ideal weight, an inability to take oral food or fluids within 7 days post surgery, and hypercatabolic situations such as major infection with fever. TPN solutions requires water (30 to 40 mL/kg/day), energy (30 to 45 kcal/kg/day, depending on energy expenditure), amino acids (1.0 to 2.0 g/kg/day, depending on the degree of catabolism), essential fatty acids, electrolytes, vitamins, minerals, and trace elements. These solutions can be adjusted, depending on the presence of organ system impairment or the specific nutritional needs of the client. TPN is usually used in hospital, subacute and long-term care, but it is also used in the home care settings.
The major goals for the patient undergoing total parental nutrition may include improvement of nutritional status, maintaining fluid balance, and absence of complications.
Here are four (4) total parenteral nutrition nursing care plans (NCP):
Imbalanced Nutrition: Less Than Body Requirements: Intake of nutrients insufficient to meet metabolic needs.
May be related to
Possibly evidenced by
Desired Outcomes
| Nursing Interventions | Rationale |
|---|---|
| Assess skin integrity and wound healing. | Skin integrity changes and wound healing are used as parameters in monitoring the effectiveness of TPN therapy. |
| Measure intake and output accurately; Monitor weight daily; Monitor calorie counts, including calories provided by TPN. | TPN composition is based on the calculated nutritional needs of the client. Before the therapy is started, a thorough baseline assessment will be completed by health care members which include physicians, nurses, dieticians, and pharmacists is done. Changes in fluid balance, weight, and caloric intake are used to assess TPN effectiveness. Daily weights are done to determine if nutritional goals are being met. Weight is also used to assess fluid volume status. Weight gain of more than 1/2 pound per day may indicate fluid retention. |
| Assist with the insertion and maintenance of central venous or peripherally inserted central catheters (PICC). | Since the osmolality of TPN solution is high, it is administered into the vascular system using a catheter inserted into a central vein with a high-volume blood flow. The tip of the catheter is usually placed in the superior vena cava. X-ray confirmation of accurate catheter placement is necessary before TPN administration is initiated. Normal saline or other isotonic solutions may be infused through the central catheter until placement is confirmed. |
| Encouraged additional oral fluid intake as indicated. | Additional oral fluids may be given to a client receiving TPN to maximize nutritional support. Clients may benefit psychologically from having oral intake, especially at shared mealtimes with family members. |
| Administer the prescribed rate of TPN solution via an infusion pump. | Electronic infusion pumps are used during the therapy to maintain an accurate rate of administration. A delayed administration time of TPN withholds the client of needed nutrition; Rapid administration can precipitate a hyperglycemic crisis because the hormonal response (i.e., insulin) may not be available to allow the use of the increased glucose load. |
| Collaborate with other nutritional support team, dietician, pharmacy, home health nurse. | The risk for most complications that occur in the hospital is decreased when the administration of parenteral nutrition is supervised by an experienced nutritional support team. |
Tin tức mới nhất
Sử dụng paracetamol dạng truyền tĩnh mạch (1 gram/100 mL)
DỰ THẢO VĂN KIỆN ĐẠI HỘI ĐẠI BIỂU KHÓA III, NHIỆM KỲ 2024 -2029
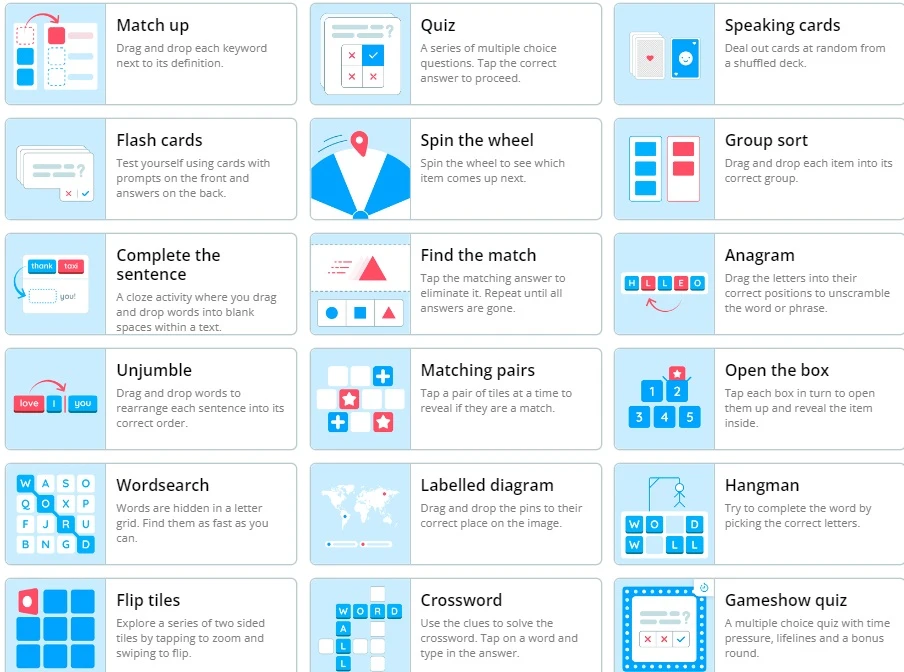
Wordwall là một công cụ dạy học trực tuyến
2 Diagnostics infirmiers NANDA 2021 -2023

Kỷ yếu hội nghị Điều dưỡng Bệnh viện HN Việt Đức 2022
Sample size calculator
Nghiên cứu bắt đầu từ đâu
Học thống kê với Dr Nuc
Hồi quy và tương quan
học Spss
địa chỉ open journal

Phần mềm điện thoại nursing